Diagnosed with patellofemoral pain syndrome? Before you do anything, make sure you understand these 9 things! There are certain movements like squats, going up and down the stairs, and jumping that can actually increase your pain. It is so important to know the best treatments for patellofemoral pain syndrome because it can actually lead to knee osteoarthritis if you don’t correct your deficits contributing to your pain.
“My knees are making these weird noises when I squat down or go down the stairs and I am so scared I am making my knee worse. What movements should I be avoiding?”
“The pain in the front of my knee flares up when I run and I was told I had patellofemoral pain syndrome. Does this mean I have to give up running?”
“I have such a hard time squatting down because I feel pressure and pain right behind my knee cap. How do I know if I have patellofemoral pain syndrome?”
These are common questions that tend to arise when someone hears they have what is called patellofemoral pain syndrome, also known as PFPS.
It can be scary and overwhelming at first. But it is important to know one thing, with the right action- you can overcome this, likely without any surgeries or procedures!
1. How does one get patellofemoral pain syndrome?
Patellofemoral pain syndrome usually occurs in a few different scenarios. Keep in mind there are other circumstances in which it can happen but these are the main ones:
- You have decreased thigh (or quad) strength that allows your knee cap to become a little unstable. This moves it out of its groove that it likes and can aggravate it.
- You increase your activity suddenly– i.e running a race with little training, going up and down a bunch of stairs, or do a lot of something your body is not used to. This can anger your kneecap.
- You have something called “pes pronatus” which means you have a fallen arch in your foot or feet that can change how your knee and hip move- thus creating stress at the kneecap.
You may fall in one or a couple of these categories, as this condition is likely caused by a mix of things.
It is important to decipher at least one main reason that contributed to your recent increase in pain because you will then use that to find out what to focus on for treatment.
2. What are the symptoms?
Typical symptoms include:
- Anterior knee pain or pain in the front of your knee
- Minor swelling
- Pain with squatting (present in up to 80% of cases)
- Pain and/or stiffness when moving the knee after sitting for prolonged period of time
Catching and locking, history of trauma, pain on the bone, and pain directly on the patella are not usually consistent with this condition.
3. What typically makes The condition worse?
With this diagnosis, you likely are experiencing some pain or feeling of pressure behind your knee cap or around your knee cap. There may be some slight swelling but significant swelling and/or warmth may indicate something else is going on.
If you have patellofemoral pain syndrome, likely these activities will not feel very good to you:
- squatting
- going up and/or down stairs
- running
- jumping
Anything where you are putting weight through a bent knee, will likely cause irritation which you do in each one of these above activities.
When first starting to heal from this condition, it is ideal to find movements you can do that don’t flare up your pain. You don’t want to constantly irritate the knee cap.
This is by no means saying you can never do these activities again, you just have to allow for the irritation to calm down before returning.
4. Are the knee noises you hear normal?
Knee noises or crepitus can be common with patellofemoral pain syndrome because if your kneecap isn’t sliding in the nice, smooth groove- it can get a little rough.
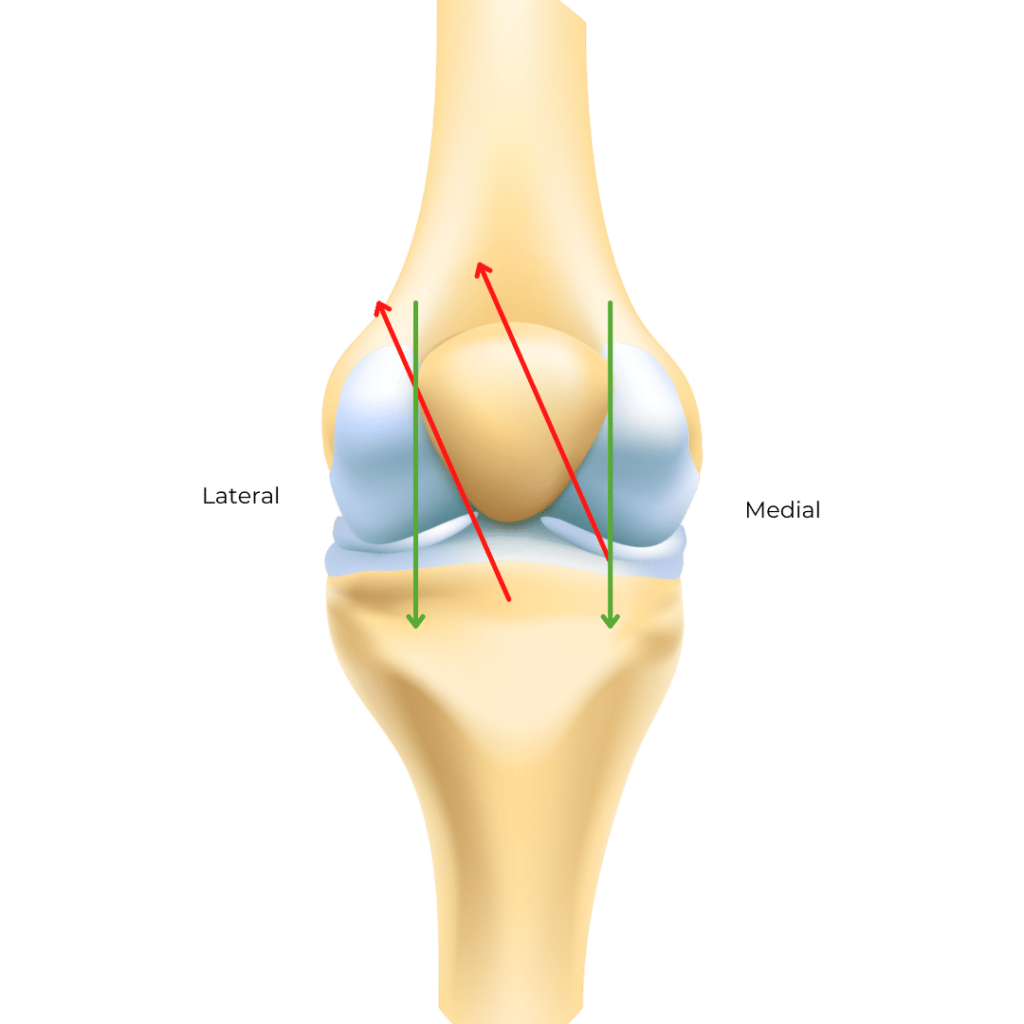
For example, in the picture, you see the green arrows indicate the direction the kneecap is supposed to move in. There is a smooth groove called the trochlear groove it travels up and down in.
The red arrows indicate an instance where the kneecap is pulled laterally (toward the outside of your leg). Now this is usually very subtle but takes your kneecap off-roading into unfamiliar territory.
Using certain exercises and strengthening you can bring your kneecap closer to the groove which can then dampen the noise.
You can read more on knee noises here.
5. How do you decrease the pain?
You can decrease pain by finding and addressing what is irritating your kneecap.
If thigh muscle (quadriceps) weakness is flaring your pain, that needs to be addressed. You can test your strength with a straight leg raise here.
If tight hamstrings are flaring your pain, that needs to be addressed. You can test and see if your hamstrings are tight here.
If you have flat feet or a fallen arch affecting the knee and hip, that needs to be addressed. If your shoes are consistently worn down on the medial edge of the shoe, this could potentially indicate you have this. You can watch this video here for more information on how to choose the right shoe.
If you had a history of a kneecap dislocation or subluxation (where it goes out of the groove but then moves back in immediately) or if you are hypermobile (really flexible)- I recommend you seek out help from a trusted physical therapist in your area to get you on the right path to strengthening
6. Can you run, jump, and squat again?
The answer is most likely yes if you reduce your pain and get strong in the right areas. Unfortunately the pain won’t magically go away.
While you are reading this blog post, you are taking a step in the right direction!
It is critical to make sure your joints are prepared for these activities again.
When you return to certain activities, you want to make sure you are doing so gradually. For example, starting with walk-run intervals when getting back to running and using an appropriate squat modification before returning to squatting with weight.
None of these activities need to be ruled out.
Clients I worked with have returned to hiking and even running with patellofemoral pain syndrome. Don’t let anyone tell you to dream small because of knee pain.
You can absolutely overcome it, you just need to make sure you are doing the right things to not only relieve pain now, but also setting yourself up for success in the future.
7. Do you need an x-ray, MRI, or other image?
Likely no.
If you have tried other things like exercise, certain anti-inflammatory medications (if prescribed or cleared by physician), and reducing painful movements without success, imaging may help reveal other causes of pain such as osteoarthritis.
MRIs usually aren’t the most helpful for patellofemoral pain syndrome because the cartilage of the kneecap isn’t typically impacted with this condition. The other things such as bone marrow lesions and fat pad inflammation you can also see, aren’t typically associated with this condition either.
If you are simply demonstrating the symptoms described above, an image likely won’t be helpful.
If you are experiencing other symptoms such as significant swelling, warmth, pain that does not resolve with exercise, morning stiffness, pain spreading to other joints, or pain that wakes you up at night, these may be signs that something else is going on.
8. What is the best treatment for patellofemoral pain syndrome?
The best treatment for patellofemoral pain is exercise. You have to make sure you do the right exercise though.
Increasing your hamstring and thigh strength helps relieve your pain but you can’t forget about. hterest of your body.
Per the research, core stability helps to improve muscle recruitment and prevent any compensations.
Hip strengthening can help to alleviate some of the stress at the knees and help with joint alignment, especially in females.
9. What are 3 exercises you should start doing?
Shown in this video below, the 3 exercises to prioritize include:
- Straight leg raise with legs elevated
- Walking backwards (with or without resistance)
- Deadlift
Take a look at the video to learn the reasoning behind each exercise!
The straight leg raise is important to help activate the quad muscle and isometrically contract it, without being overpowered by the hips. This exercise can be challenging at first.
Research has actually shown that walking backwards tends to activate more of the Vastus Medialis Oblique (VMO) muscle which is important to keep your kneecap in the groove, while also reducing joint stress.
The deadlift helps to reduce hamstring tightness through strength to support the knee joint and help it move and absorb stress how it should.
Conclusion
If you have patellofemoral pain syndrome, it is important to take the right action. It has the ability to progress into patellofemoral arthritis and knee osteoarthritis.
It is incredibly important to first start with finding movements that build strength in the right areas and can help with knee cap tracking. Make sure to focus on joints such as the hip and ankle, not just the knee with this condition. These muscles play a large role in supporting the knee and helping with alignment.
If you are looking for ways to build strength, reduce pain, and prevent the condition from increasing in severity- Adventurers for Life is the path you need.
Adventurers for Life is my signature membership that gives you the exact workouts you need to improve standing, walking, stairs, getting down to and up from the floor and even higher impact activities without aggravating your joint(s).
This step by step path can open the doors to so many adventures.
References:
Abdelraouf, Osama Ragaa et al. “Backward walking alters vastus medialis oblique/vastus lateralis muscle activity ratio in females with patellofemoral pain syndrome.” Turkish journal of physical medicine and rehabilitation vol. 65,2 169-176. 25 Apr. 2019, doi:10.5606/tftrd.2019.2445
Chevidikunnan, Mohamed Faisal et al. “Effectiveness of core muscle strengthening for improving pain and dynamic balance among female patients with patellofemoral pain syndrome.” Journal of physical therapy science vol. 28,5 (2016): 1518-23. doi:10.1589/jpts.28.1518
Gaitonde, David Y et al. “Patellofemoral Pain Syndrome.” American family physician vol. 99,2 (2019): 88-94.
Alyssa Kuhn
Disclaimer: This post is for general informational purposes only. It should not be used to self-diagnose and it is not a substitute for a medical exam, cure, treatment, diagnosis, and prescription or recommendation. It does not create a doctor-patient relationship between Dr. Kuhn and you. You should not make any change in your health regimen or diet before first consulting a physician and obtaining a medical exam, diagnosis, and recommendation. Move Well Age Well, LLC and Dr. Alyssa Kuhn, PT, DPT are not liable or responsible for any advice, course of treatment, diagnosis or any conclusions drawn, services or product you obtain through this video or site.