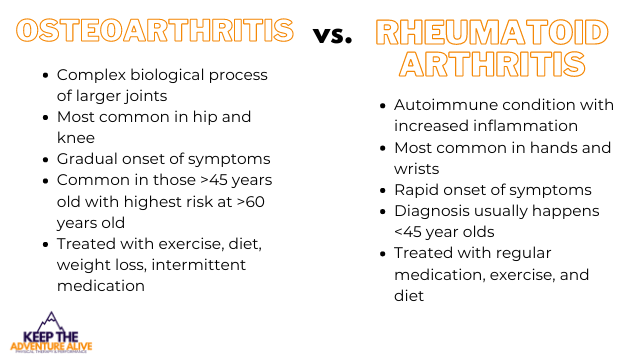
Understanding osteoarthritis vs rheumatoid arthritis is important because it can significantly impact treatment. Osteoarthritis is a complex biological disease of the contents that make up a joint, instead of the popular “wear and tear” theory, particularly in knee and hip joints. Rheumatoid arthritis is a dysfunction of the immune system that leads to increased inflammation, particularly in smaller joints. Both conditions have distinct symptoms aside from the symptoms they share including pain and functional disability. Osteoarthritis is best treated conservatively with diet, exercise, and intermittent pharmacological intervention while rheumatoid arthritis depends more heavily on pharmacological treatment. Let’s look at the differences.
How do I know the difference?
When trying to figure out if you have osteoarthritis vs rheumatoid arthritis, there are a few questions you have to ask yourself. Please bear in mind a medical professional will help you to best figure out your diagnosis.
Let’s start here:
Osteoarthritis is a condition of the joints that is exacerbated by low-grade chronic inflammation. Contrary to popular belief, osteoarthritis is NOT caused by wear and tear (watch this video to learn more). Some of the popular symptoms include joint pain, stiffness especially in the morning, and loss of range of motion. Learn more about what osteoarthritis feels like here.
Osteoarthritis commonly can affect one side compared to the other, for example one knee may be more painful than the other. Symptoms tend to stay local to the painful joint. It commonly impacts knees, hips, spine, and hands.
Rheumatoid Arthritis is an “is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body” according to the CDC.
With rheumatoid arthritis, you may experience other symptoms such as fatigue, warm joints, fever, and symptoms in joints on both sides of the body. It commonly impacts hands, feet, ankles, and knees.
Why do I need to know the difference?
If you’re dealing with joint pain that doesn’t seem to be going away, it can be so important to find a diagnosis. When looking at osteoarthritis vs rheumatoid arthritis, they are treated a little differently which can allow for different treatment plans in order to find relief.
By understanding your diagnosis, you can find answers to these questions including:
- What is causing this type of arthritis?
- What symptoms can I expect?
- What are the best ways to find pain relief?
- Do I need surgery?
It can be overwhelming to fall into this trap of trying to get all of the answers at once. There is a ton of information out there and unfortunately, our questions may remain unanswered.
This article takes the most recent evidence on both of these conditions to help you get one step closer to cracking the code of your arthritis. If your arthritis is isn’t diagnosed properly, you could be missing out on some of the best treatments! Let’s take a further look at how to differentiate osteoarthritis vs rheumatoid arthritis.
What is causing this arthritis?
When looking at the causes of osteoarthritis vs rheumatoid arthritis, controlling some of these risk factors may help to reduce the progression of the condition.
Osteoarthritis:
Risk factors for osteoarthritis include genetics, history of joint injury, the foods you eat, presence of insulin resistance, obesity, increasing age, poor sleep habits, inactivity, and/or muscular weakness. These risk factors contribute to increased levels of inflammation in the body.
As inflammation starts to collect, it can begin to wreak havoc in your body. Certain processes aren’t able to work as efficiently including cartilage building and repair. This can lead to irritation, stiffness, and increased sensitivity to pain.
It is important to note that osteoarthritis is not inevitable with increasing age. Certain factors associated with getting older increase your risk of developing osteoarthritis but do not guarantee it.
You can also have what’s called secondary osteoarthritis, which is joint damage secondary to a pre-existing condition that impacts the joints. It’s “predisposing conditions include trauma or injury, congenital joint disorders, inflammatory arthritis, avascular necrosis, infectious arthritis, Paget disease, osteopetrosis, osteochondritis dissecans, metabolic disorders (hemochromatosis, Wilson’s disease), hemoglobinopathy, Ehlers-Danlos syndrome, or Marfan syndrome”.
Muscular weakness and changes in your joint structure can impact the amount of force going through certain parts of your joints. This is because these risk factors alter your mechanics and place unevenly distributed force on certain parts of your joint, initiating negative consequences.
Rheumatoid Arthritis:
Risk factors are less clear compared to osteoarthritis. It has been found that rheumatoid arthritis is primarily driven by genetics or environmental factors with genetics having a strong component in this condition.
According to researcher Krati Chauhan et al. in an article updated in 2020, “cigarette smoking is the strongest environmental risk factor associated with rheumatoid arthritis. Studies have shown in ACPA (anti-citrullinated protein antibody) positive individuals; there is an interaction between genes and smoking that increases the risk of RA”.
What Symptoms to expect
Knowing the symptoms of osteoarthritis vs rheumatoid arthritis can help you to begin to narrow down what is causing your pain. Please note that you can actually have a cross-over of both conditions so if you are experiencing symptoms of both, please consult a doctor or rheumatologist.
Osteoarthritis
Common symptoms of osteoarthritis include joint stiffness, localized joint pain, impaired balance, joint instability- buckling or giving way, occasional swelling, and limited range of motion.
These symptoms typically have a gradual onset. The symptoms may be most apparent in knees, hips, spine, or hands. It is possible to have osteoarthritis in multiple joints.
Here are a couple of statistics about the joints typically affected by osteoarthritis from Zhang et al.:
“The age-standardized prevalence of symptomatic hand and knee OA is 6.8% and 4.9%, respectively, in Framingham subjects age ≥26 years.”
“However, prevalence of symptomatic knee OA was 16.7% among subjects age ≥45 in the Johnston County Osteoarthritis Project, much higher than that reported in the Framingham Study.”
“About 9% of subjects in the Johnston County study had symptomatic hip OA”
Gradually increasing pain in knee, hands, and/or hips with stiffness in the morning along with occasional swelling and instability, there is a chance you may have osteoarthritis. It is important to note that everyone has a different experience with osteoarthritis so these symptoms could vary.
This post “What Does Osteoarthritis Feel Like” expands on the 4 most common symptoms.
Osteoarthritic joints can experience occasional flare ups which are usually triggered by overactivity but can also be influenced by the weather, especially cold temperatures or humidity.
These flare ups typically include increased joint pain, increased joint swelling, and higher degree of stiffness.
Rheumatoid Arthritis:
Compared to osteoarthritis, you may notice a quicker onset of symptoms that primarily affect your hands, but can also affect wrists, elbows, shoulders, ankles, and knees.
You may also nodules that form on your joints in your fingers or toes, as they are found in 20% of the cases of rheumatoid arthritis.
In the joints described above, you may notice swelling, redness, and warmth as well as prolonged joint stiffness that typically lasts longer than osteoarthritis.
These symptoms usually occur at younger ages and usually affect multiple joints at once. This is compared to osteoarthritis which starts typically with 1-2 joints with a slower progression.
According to the Arthritis Foundation, pain flare ups are common with rheumatoid arthritis and can be debilitating. These flare ups include increased joint pain, increased swelling, and overall fatigue. A participant in a focus group described pain felt during a flare up as “…doesn’t let up. It just is unrelenting.” Severity and frequency does depend on the person.
These flare ups can be triggered by overactivity, not getting enough sleep, or followed by an infection such as a cold or flu.
Fatigue, nausea, fever, and other systemic symptoms may be present due to the autoimmune nature of the condition. It can affect different organs and lead to other symptoms aside from pain and stiffness.
How they are diagnosed
Knowing the diagnosis process can help you to understand what you will need to go through for a diagnosis and maybe what has been missed so far.
Osteoarthritis
Osteoarthritis can be characterized into 5 different stages.
According to Rouhin et al, “OA is a clinical diagnosis and can be diagnosed with confidence if the following are present:
1) pain worse with activity and better with rest
2) age > 45 years
3) morning stiffness lasting less than 30 minutes
4) bony joint enlargement
5) limitation in range of motion”
Osteoarthritis is typically diagnosed with ruling out other conditions such as other types of arthritis.
X-rays can show some degree of osteoarthritis but is not always the most accurate because research has shown that even with arthritic changes on an x-ray, people could be totally asymptomatic.
You may also want to have your C-reactive protein levels (CRP) tested as they can be elevated in osteoarthritis as it indicates systemic inflammation.
Rheumatoid Arthritis
In accordance with the symptoms, there is a blood test that can be done for rheumatoid arthritis that tests for something called the rheumatoid factor. It has been found that “about 45% to 75% of patients with rheumatoid arthritis test positive for rheumatoid factor.”
Presence of the rheumatoid factor doesn’t necessarily guarantee rheumatoid arthritis. It may be worth also testing for “Acute-phase reactants, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be elevated in the active phase of arthritis.”
X-rays may not be the most helpful for rheumatoid arthritis, especially in the early stages. In more advanced stages, some erosion and other joint changes may be observable.
What are the best forms of treatment?
Treatments do differ with osteoarthritis vs rheumatoid arthritis so it is important to get a clear diagnosis of what condition you have.
Osteoarthritis
The best course of treatment for osteoarthritis includes managing pain through controlling inflammation. This is best done by:
- weight reduction to decrease inflammation associated with fat tissue
- increasing exercise movements that do not flare up pain. Exercise actually is one of the BEST ways to manage osteoarthritis compared to popular belief, learn more here.
- adopting an anti-inflammatory diet such as the Mediterranean diet. Find the best anti-inflammatory foods list here.
- medications for pain flare ups or uncontrolled pain including topical or oral non-steroidal anti-inflammatory drugs (NSAIDS). Duloxetine has also been shown to be an alternative if you are unable to take NSAIDs.
- use of pain relieving compression braces (here are our favorites for the knee!)
Rheumatoid Arthritis
It has been found that “the early use of disease-modifying anti-rheumatic drugs (DMARDs) and biologics is more effective than treatment with glucocorticoids and NSAIDs” is one of the best treatments for rheumatoid arthritis. In order to get the maximum benefit of pain relief, it is necessary to supplement with other inflammation fighting behaviors such as diet and exercise.
Joint stiffness is a large part of rheumatoid arthritis and finding the right movements can be extremely effective in fighting joint stiffness almost immediately. The trick is finding the right movements that won’t flare up pain.
There are potentials for joint replacement surgeries with rheumatoid arthritis too, with knee replacements being the most common.
According to the Rheumatology network, researchers found that:
• After hip or knee replacement, patients with rheumatoid arthritis (RA) had lower rates of joint revision surgery than patients with osteoarthritis.
• However, patients with RA had higher rates of death and prosthetic joint infections following hip or knee replacement compared with patients with osteoarthritis (1.6% of patients with RA experienced an infection compared to the 1% with osteoarthritis).
Osteoarthritis vs rheumatoid arthritis checklist
When looking at osteoarthritis vs rheumatoid arthritis consider the following:
- Which joints are primarily affected?
- Does your morning joint stiffness last longer that 60-90 minutes?
- What is your age?
- Does rheumatoid arthritis or osteoarthritis run in your family?
- Did your symptoms appear fast or slowly over time?
- Do you experience fatigue, nausea, or a fever with your flares?
RECAP: Osteoarthritis vs rheumatoid arthritis
Remember larger joints tend to be impacted by osteoarthritis (knee, hip, spine) while rheumatoid arthritis impacts smaller joints (hands, ankles, toes, shoulders, with some exceptions for larger joints like knees).
Morning stiffness that lasts longer than 90 minutes may be indicative of rheumatoid arthritis whereas osteoarthritis morning stiffness usually can go away in 20-30 minutes with movement.
Younger <45 people tend to be affected by rheumatoid arthritis where as osteoarthritis typically occurs in those >45 years with the highest risk >60.
Both have a genetic component.
If your symptoms appeared more quickly, it could be indicative of rheumatoid arthritis due to the autoimmune nature of the condition. Osteoarthritis symptoms tend to develop over time.
Experiencing other systemic symptoms may point to rheumatoid arthritis. Fatigue could be a symptom of osteoarthritis too due to poor sleeping habits.
Next steps:
If you suspect you have osteoarthritis- seeking out care from an osteoarthritis specialist is vital. Here are some tips on how to find one. From there you can create a plan including the best ways to manage inflammation so you can live out your adventure!
If you are having a hard time finding someone you trust that listens to your goals, don’t sell yourself short. I believe your arthritis adventure is absolutely possible.
If you suspect rheumatoid arthritis, you could start with your primary care physician but it may be a good idea to seek out a rheumatologist as they are specialists in inflammatory conditions like rheumatoid arthritis.
If you are looking for weekly arthritis tips and tricks sent to your inbox, sign up for the free newsletter HERE.
Disclaimer: This post is for general informational purposes only. It should not be used to self-diagnose and it is not a substitute for a medical exam, cure, treatment, diagnosis, and prescription or recommendation. It does not create a doctor-patient relationship between Dr. Kuhn and you. You should not make any change in your health regimen or diet before first consulting a physician and obtaining a medical exam, diagnosis, and recommendation. Move Well Age Well, LLC and Dr. Alyssa Kuhn, PT, DPT are not liable or responsible for any advice, course of treatment, diagnosis or any conclusions drawn, services or product you obtain through this video or site.